Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
Information handout only (PDF)
A copy of the information handout in PDF format.
This professional resource aids mental health practitioners during the eye movement desensitization and reprocessing (EMDR) assessment phase by offering a list of negative and positive cognitions commonly associated with traumatic memories.
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
A copy of the information handout in PDF format.
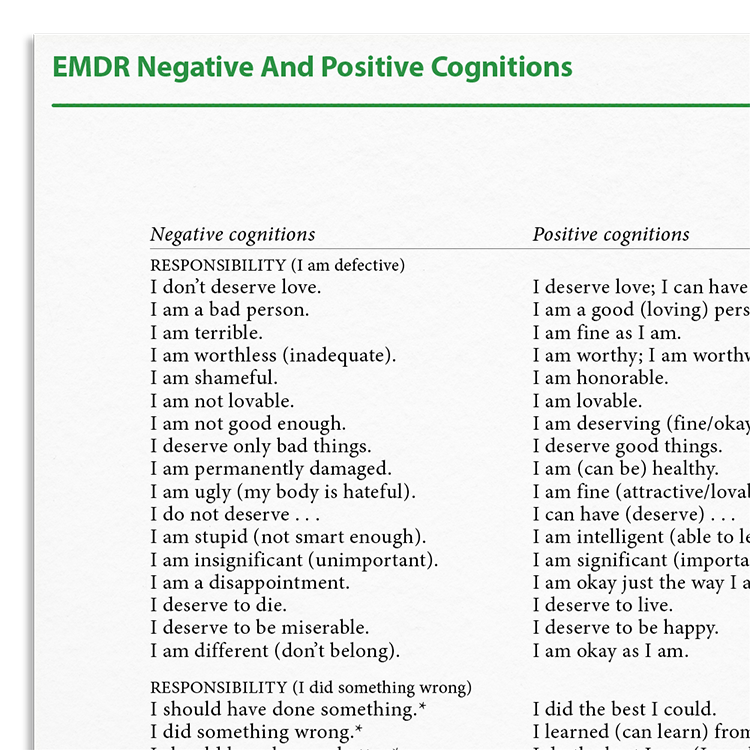
The EMDR Negative And Positive Cognitions Information Handout is a practical tool designed for use during Phase 3 of the EMDR protocol. In this phase, therapists support clients in identifying negative self-beliefs linked to a target memory, along with preferred positive cognitions that support adaptive reprocessing. This handout can be especially helpful when clients struggle to articulate their beliefs. By offering a structured list of commonly reported cognitions, it provides language options that can support the EMDR assessment process.
Exploration of beliefs and cognitions is a key component in several EMDR phases, particularly during assessment and installation. This handout:
Identifying beliefs associated with unresolved trauma.
Use the handout to support clients in exploring negative and positive cognitions associated with a chosen target memory.
Help clients distinguish between their current negative beliefs and preferred positive beliefs linked to their traumatic experience.
Use the VoC (Validity of Cognition) and SUDs (Subjective Units of Distress) scales to evaluate the intensity of beliefs and related emotional responses.
This resource is grounded in the Adaptive Information Processing (AIP) model, which underpins eye movement desensitisation and reprocessing (EMDR) therapy. According to the AIP model, dysfunctionally stored memories can give rise to maladaptive beliefs and present-day symptoms. EMDR aims to access and reprocess these memories so that more adaptive information can be integrated.
Phase 3 of the EMDR protocol — the Assessment Phase — involves identifying a target memory along with a linked negative cognition (NC) and a preferred positive cognition (PC). This process activates relevant memory networks and lays the groundwork for reprocessing and installation.
Some clients, particularly those with complex or developmental trauma histories, may struggle to articulate their beliefs. A structured list of commonly observed cognitions can serve as a helpful tool, offering language that resonates with the client’s internal experience and supporting a more focused, collaborative assessment process.
Just enter your name and email address, and we'll send you EMDR Negative And Positive Cognitions (English US) straight to your inbox. You'll also receive occasional product update emails wth evidence-based tools, clinical resources, and the latest psychological research.
Working...
This site uses strictly necessary cookies to function. We do not use cookies for analytics, marketing, or tracking purposes. By clicking “OK”, you agree to the use of these essential cookies. Read our Cookie Policy