1st November 2022 Newsletter

Psychology Tools
Published
Welcome to the November 2022 newsletter. We have devoted this month’s edition entirely to body dysmorphic disorder (BDD). BDD is common (population prevalence of 1 – 3%), but is often not disclosed due to shame and embarrassment. Many clinicians are unfamiliar with contemporary treatment approaches. This month we’re pleased to announce the release of three new BDD resources, as well as our research roundup, focusing on the latest BDD research.
New Releases

Understanding Body Dysmorphic Disorder
This is a friendly, comprehensive and explanatory guide written for clients, but it’s equally useful as a scaffold for clinicians. It includes:
How to recognize symptoms of BDD and its causes.
An introduction to body image.
A deep dive into the maintenance of BDD, including ‘zooming in’ on body image concerns, appearance/checking rituals, and unhelpful cognitive processes.
An introduction to contemporary treatment approaches for BDD and what they might involve, with vignettes and examples.

What Is Body Dysmorphic Disorder (BDD)?
Many people have concerns about how they look, but significant and persistent worry about one’s appearance may be a sign of body dysmorphic disorder (BDD). BDD centres on an individual’s belief (or felt sense) that there is something wrong with the way they look. This handout explains what BDD is, what maintains it, and what the recommended treatments are.
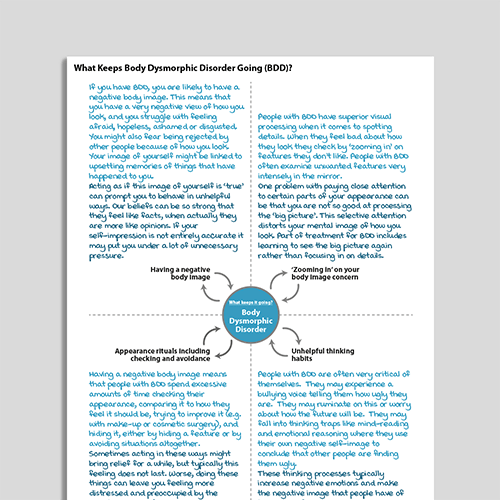
What Keeps Body Dysmorphic Disorder (BDD) Going?
The “What Keeps It Going?” series is a set of one-page diagrams explaining how common mental health conditions are maintained. Friendly and concise, they provide an easy way for clients to understand at a glance why their disorders persist, and how they might be interrupted. What Keeps Body Dysmorphic Disorder (BDD) Going? is designed to help clients experiencing BDD understand more about their condition.
Latest Research

Clinical guidance on the treatment of BDD (2021)
If you want to read just one thing to refresh your knowledge of BDD, make it this one.
The International College of Obsessive-Compulsive Spectrum Disorders (www.ICOCS.org) is a global network of expert clinicians, researchers, and ‘experts by experience of OCD’. In recognition of the need for updated clinical guidance on the treatment of BDD the ICOCS and OCRN have developed this treatment synthesis, based on expert consensus. Briefly, the recent advances in the field have been selected by a range of experts who have considered those of most relevance to the management of BDD.
Castle, D., Beilharz, F., Phillips, K. A., Brakoulias, V., Drummond, L. M., Hollander, E., … & Fineberg, N. A. (2021). Body dysmorphic disorder: a treatment synthesis and consensus on behalf of the International College of Obsessive-Compulsive Spectrum Disorders and the Obsessive Compulsive and Related Disorders Network of the European College of Neuropsychopharmacology. International Clinical Psychopharmacology, 36(2), 61.

Predictors and moderators of symptom change in BDD
Highlights of this study, and areas on which clinicians can focus when delivering CBT for BDD, include:
Several variables predict therapy outcomes for body dysmorphic disorder.
Greater treatment credibility predicts greater improvement with therapy.
Obsessive-compulsive personality disorder predicts greater improvement with therapy.
Baseline SRI treatment (unchanged during the study) predicts less improvement.
Phillips, K. A., Greenberg, J. L., Hoeppner, S. S., Weingarden, H., O’Keefe, S., Keshaviah, A., … & Wilhelm, S. (2021). Predictors and moderators of symptom change during cognitive-behavioral therapy or supportive psychotherapy for body dysmorphic disorder. Journal of affective disorders, 287, 34-40.
Get sent more useful pieces like this!
Sign up to our monthly newsletter full of helpful ideas, tools, and tips for mental health professionals like you. You'll find out about our latest resources, and you can also read our reviews of the latest research.
It's completely free and you can unsubscribe at any time.