Body Dysmorphic Disorder (BDD)
Body Dysmorphic Disorder (BDD) is a mental health condition characterized by an excessive preoccupation with perceived flaws in physical appearance, which are either unnoticeable or appear minor to others. This preoccupation often leads to significant distress, impaired functioning, and repetitive behaviors such as mirror-checking, camouflaging, or seeking reassurance. BDD can severely impact an individual’s quality of life, social interactions, and mental well-being. Evidence-based treatments, such as cognitive behavioral therapy (CBT) and pharmacotherapy, have shown effectiveness in managing symptoms and improving outcomes.
Showing 1 to 19 of 19 results
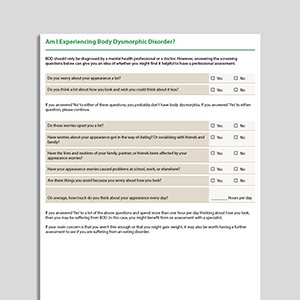
Am I Experiencing Body Dysmorphic Disorder (BDD)?
Am I Experiencing Body Dysmorphic Disorder (BDD)?
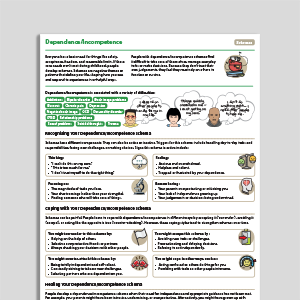
Disqualifying The Positive
Disqualifying The Positive
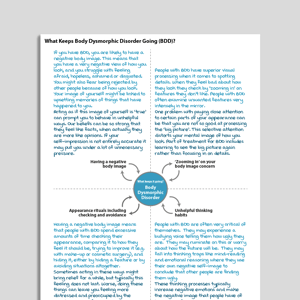
What Keeps Body Dysmorphic Disorder (BDD) Going?
What Keeps Body Dysmorphic Disorder (BDD) Going?
Understanding Body Dysmorphic Disorder
Understanding Body Dysmorphic Disorder
Recognizing Body Dysmorphic Disorder
Recognizing Body Dysmorphic Disorder
What Is Body Dysmorphic Disorder (BDD)?
What Is Body Dysmorphic Disorder (BDD)?
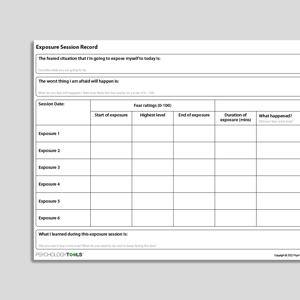
Exposure And Response Prevention
Exposure And Response Prevention
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)
Links to external resources
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
Assessment
-
Body Image Questionnaire (BIQ)
| Veale | 2009
- Scale
- Cosmetic Procedure Screening Questionnaire (COPS) | Veale | 2009
- Body dysmorphic disorder screening tools for the dermatologist: A systematic review | Danesh, M, Beroukhim, K., Nguyen, C., Levin, E., & Koo, J. | 2015
Information Handouts
- What is Body Dysmorphic Disorder? | Centre For Clinical Interventions
- What is body dysmorphic disorder? | IOCDF: Fugen Neziroglu, Jill C. Slavin
Presentations
- Body Dysmorphic Disorder (BDD) and Muscle Dysmorphia | Nicole Schnackenberg, Alex Mummery | 2019
Self-Help Programmes
-
Building Body Acceptance
| Centre For Clinical Interventions | 2012
- Module 1: Understanding Body Dysmorphic Disorder
- Module 2: What keeps BDD going?
- Module 3: Reducing Appearance Preoccupation
- Module 4: Reducing Checking And Reassurance Seeking
- Module 5: Overcoming Negative Predictions, Avoidance & Safety Behaviors
- Module 6: Adjusting Appearance Assumptions
- Module 7: Self-Management Planning
-
Caring Less About Your Looks
| Centre For Clinical Interventions | 2019
- Module 1: The Impact Of Appearance Overconcern
- Module 2: What Keeps Appearance Concerns Going
- Module 3: Appearance Focused Attention
- Module 4: Body Checking And Reassurance Seeking
- Module 5: Appearance Altering Behaviors
- Module 6: Avoidance And Safety Behaviors
- Module 7: Overvaluing Appearance And Self-Management Planning
Treatment Guide
- NICE Guidelines For OCD and BDD | NICE | 2005
What Is Body Dysmorphic Disorder?
BDD involves a persistent and distressing preoccupation with perceived defects or flaws in physical appearance. According to DSM-5 criteria, it includes:
A preoccupation with one or more perceived physical defects that are not observable or appear slight to others.
Repetitive behaviors (e.g., mirror-checking, skin-picking, excessive grooming) or mental acts (e.g., comparing appearance to others) in response to appearance concerns.
Significant distress or impairment in social, occupational, or other areas of functioning.
The disturbance is not better explained by concerns related to body fat or weight in the context of an eating disorder.
ICD-11 criteria similarly describe BDD as a disorder marked by excessive concern about a perceived physical flaw, often associated with repetitive behaviors or mental acts aimed at addressing these concerns.
Incidence and Risk Factors
BDD affects approximately 2–3% of the general population, with men and women affected at similar rates (Phillips et al., 2006). It often emerges during adolescence, a time of heightened self-consciousness and physical changes.
Key risk factors include:
Genetic predisposition: Research indicates that genetics can play a role in BDD (e.g., Enander et al., 2018). Family history of OCD or anxiety disorders may increase susceptibility (e.g., Brakoulias et al., 2011).
Cognitive vulnerabilities: Perfectionism, low self-esteem, and a heightened focus on appearance can contribute to the development of BDD (Veale et al., 2016).
Sociocultural influences: Societal pressures emphasizing idealized beauty standards and exposure to social media may play a role in exacerbating concerns about appearance (Dixon & Marques, 2017).
Early life experiences: Bullying, teasing, or trauma related to appearance during childhood or adolescence can contribute to the development of BDD (Monzani et al., 2024).
Psychological Models and Theories
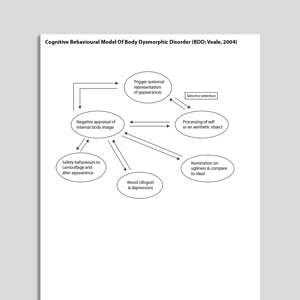
The cognitive behavioral model suggests that BDD is maintained through distorted beliefs about appearance, heightened self-focused attention, and maladaptive coping behaviors (Veale, 2004). Individuals with BDD often overestimate the importance of physical appearance in determining their self-worth and assume others scrutinize their perceived flaws.
The Tripartite Influence Model, or sociocultural model, of body dysmorphic disorder (Thompson et al, 1999) explains how societal beauty standards contribute to body dissatisfaction through influences from peers, family, and media, including social media. These sources expose individuals to idealized body norms, which are internalized and lead to self-comparisons. Comparing oneself to these ideals often results in negative evaluations of one’s own body, fostering body dissatisfaction. This dissatisfaction can contribute to psychological distress, disordered eating, and appearance-related concerns, including those seen in Body Dysmorphic Disorder (BDD).
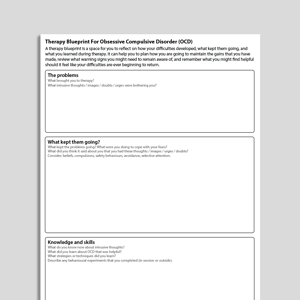
Evidence-Based Psychological Approaches for BDD
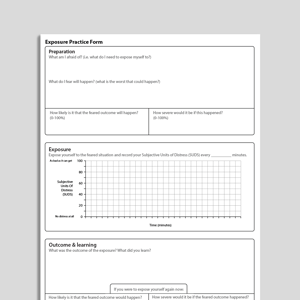
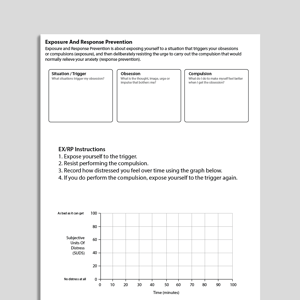
Cognitive Behavioral Therapy (CBT) is an effective psychological treatment for BDD according to several studies (Harrison et al., 2016). It focuses on challenging distorted beliefs about appearance, reducing repetitive behaviors and self-focused attention, and improving emotional regulation. Techniques such as exposure and response prevention (ERP) help individuals confront avoided situations and resist compulsive behaviors (Veale & Neziroglu, 2010). Research demonstrates significant improvement in mood- and BDD-related symptoms following treatment (Harrison et al., 2016; Wilhelm et al., 2014).
Pharmacotherapy. Selective serotonin reuptake inhibitors (SSRIs) are often used in conjunction with psychotherapy. They have been shown to reduce obsessive thoughts and compulsive behaviors associated with BDD, particularly in moderate to severe cases (Phillips et al., 2002).
Mindfulness-Based Interventions:
Mindfulness practices encourage individuals to focus on the present moment and develop a nonjudgmental awareness of their thoughts and feelings. These interventions can reduce self-focused attention and promote self-acceptance. Research suggests that mindfulness-based might be useful for people with BDD (Gu & Zhu, 2023).
Acceptance and Commitment Therapy (ACT)
aims to help individuals accept appearance-related thoughts and feelings without judgment while focusing on value-driven actions. By promoting psychological flexibility, ACT seeks to reduce the impact of appearance concerns on daily life (Harrison et al., 2016). While some early research suggests ACT may have potential benefits for aspects of Body Dysmorphic Disorder (BDD), such as reducing shame (Linde et al., 2023), the evidence remains limited and requires further investigation to establish its effectiveness.
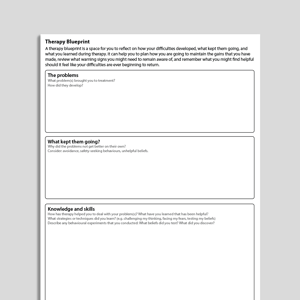
Resources for Working with Body Dysmorphic
DisorderPsychology Tools offers a variety of resources to support individuals with BDD, including:
Psychoeducational handouts on understanding and managing BDD.
Cognitive behavioral models and worksheets for addressing distorted thoughts and beliefs.
Exposure and response prevention resources suitable for BDD-related behaviors.
Information and exercises for addressing selective attention.
Mindfulness exercises to reduce self-focused attention and promote self-compassion.
Compassion-focused resources to reduce shame and self-criticism.
References and Further Reading
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). APA.
Brakoulias, V., Starcevic, V., Sammut, P., Berle, D., Milicevic, D., Moses, K., & Hannan, A. (2011). Obsessive-compulsive spectrum disorders: a comorbidity and family history perspective. Australasian Psychiatry, 19, 151-155.
Dixon, L., & Marques, L. (2017). Cultural, racial, and ethnic aspects of body dysmorphic disorder and treatment implications. In K. Phillips (Ed.), Body dysmorphic disorder: Advances in research and clinical practice (pp. 195–201). Oxford University Press.
Enander, J., Ivanov, V. Z., Mataix-Cols, D., Kuja-Halkola, R., Ljótsson, B., Lundström, S., ... & Rück, C. (2018). Prevalence and heritability of body dysmorphic symptoms in adolescents and young adults: A population-based nationwide twin study. Psychological Medicine, 48, 2740-2747.
Gu, Y. Q., & Zhu, Y. (2023). A randomized controlled trial of mindfulness-based cognitive therapy for body dysmorphic disorder: Impact on core symptoms, emotion dysregulation, and executive functioning. Journal of Behavior Therapy and Experimental Psychiatry, 81, 101869.
Harrison, A., & Cantor, A. (2016). ACT for body dysmorphic disorder: Reducing appearance concerns through psychological flexibility. Journal of Contextual Behavioral Science, 5(4), 254–260.
Harrison, A., de la Cruz, L. F., Enander, J., Radua, J., & Mataix-Cols, D. (2016). Cognitive-behavioral therapy for body dysmorphic disorder: A systematic review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 48, 43-51.
Linde, J., Luoma, J. B., Rück, C., Ramnerö, J., & Lundgren, T. (2023). Acceptance and compassion-based therapy targeting shame in body dysmorphic disorder: A multiple baseline study. Behavior Modification, 47, 693-718.
Monzani, B., Luxton, R., Jassi, A., & Krebs, G. (2024). Adverse childhood experiences among adolescents with body dysmorphic disorder: frequency and clinical correlates. Clinical Psychology and Psychotherapy, 31, e3028.
Phillips, K. A., & Hollander, E. (2006). Body dysmorphic disorder: Clinical features and treatment options. Journal of Clinical Psychiatry, 67(8), 1196–1204.
Phillips, K. A., Menard, W., Fay, C., & Weisberg, R. (2002). Psychosocial functioning and quality of life in body dysmorphic disorder. Comprehensive Psychiatry, 46(4), 254–260.
Thompson, J. K., Heinberg, L. J., Altabe, M., and Tantleff-Dunn, S. (1999). Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance. Washington, DC: American Psychological Association. doi: 10.1037/10312-000
Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image, 1, 113-125.
Veale, D., & Neziroglu, F. (2016). Body dysmorphic disorder: A treatment manual. Wiley.
Wilhelm, S., Phillips, K. A., & Steketee, G. (2014). Cognitive-behavioral therapy for body dysmorphic disorder. Guilford Press.