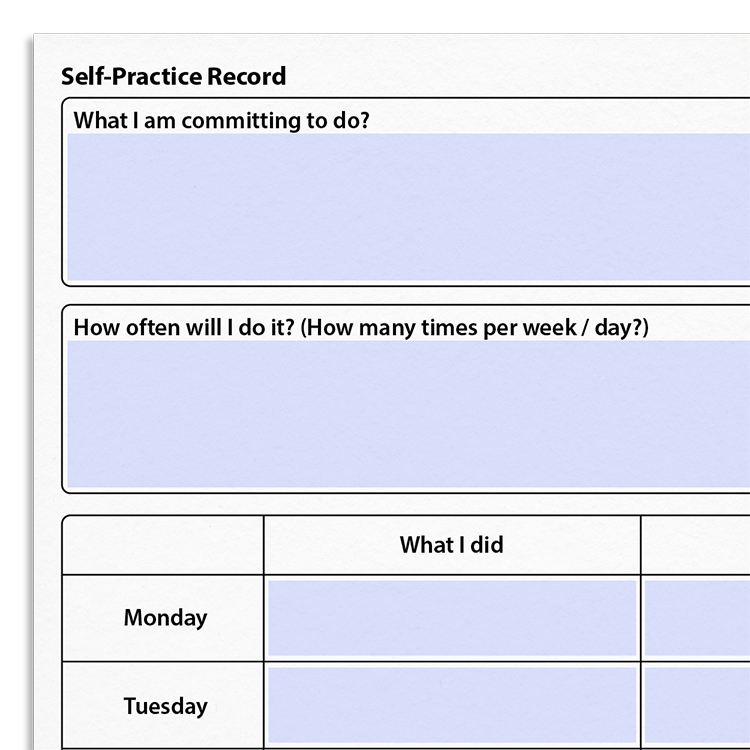
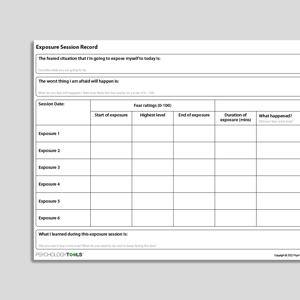
Professional version
Offers theory, guidance, and prompts for mental health professionals. Downloads are in Fillable PDF format where appropriate.
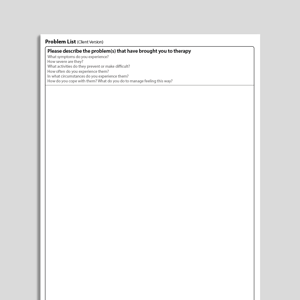
Client version
Includes client-friendly guidance. Downloads are in Fillable PDF format where appropriate.
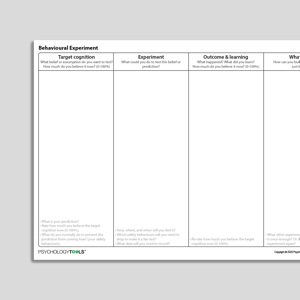
Fillable version (PDF)
A fillable version of the resource. This can be edited and saved in Adobe Acrobat, or other PDF editing software.
Editable version (PPT)
An editable Microsoft PowerPoint version of the resource.