Obsessive Compulsive Disorder (OCD) including Body Dysmorphic Disorder (BDD)
Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts, images, urges, or impulses that are interpreted as threating (obsessions). These lead to active and counterproductive attempts to reduce the thoughts and/or discharge the perceived responsibility associated with them (compulsions). Cognitive and behavioral approaches including exposure, response prevention, and behavioral experiments are effective treatments for OCD. This page also includes resources for body dysmorphic disorder (BDD).
Insufficient Self-Control
Insufficient Self-Control
Dependence / Incompetence
Dependence / Incompetence
Approval-/Admiration-Seeking
Approval-/Admiration-Seeking
Cognitive Distortions – Unhelpful Thinking Styles (Common)
Cognitive Distortions – Unhelpful Thinking Styles (Common)
Cognitive Distortions – Unhelpful Thinking Styles (Extended)
Cognitive Distortions – Unhelpful Thinking Styles (Extended)
Urges – Self-Monitoring Record
Urges – Self-Monitoring Record
Disqualifying The Positive
Disqualifying The Positive
Am I Experiencing Obsessive Compulsive Disorder (OCD)?
Am I Experiencing Obsessive Compulsive Disorder (OCD)?
Understanding Body Dysmorphic Disorder
Understanding Body Dysmorphic Disorder
What Keeps Body Dysmorphic Disorder (BDD) Going?
What Keeps Body Dysmorphic Disorder (BDD) Going?
Recognizing Obsessive Compulsive Disorder (OCD)
Recognizing Obsessive Compulsive Disorder (OCD)
What Is Body Dysmorphic Disorder (BDD)?
What Is Body Dysmorphic Disorder (BDD)?
Treating Your OCD With Exposure And Response (Ritual) Prevention (Second Edition): Workbook
Treating Your OCD With Exposure And Response (Ritual) Prevention (Second Edition): Workbook
Exposure And Response (Ritual) Prevention For Obsessive Compulsive Disorder (Second Edition): Therapist Guide
Exposure And Response (Ritual) Prevention For Obsessive Compulsive Disorder (Second Edition): Therapist Guide
Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm: Workbook
Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm: Workbook
Cognitive Behavioral Treatment Of Childhood OCD: It's Only A False Alarm: Therapist Guide
Cognitive Behavioral Treatment Of Childhood OCD: It's Only A False Alarm: Therapist Guide
Self-Monitoring Record (Universal)
Self-Monitoring Record (Universal)
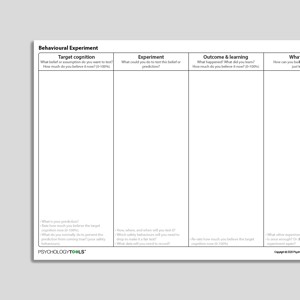
Uncertainty Beliefs – Experiment Record
Uncertainty Beliefs – Experiment Record
What Keeps Obsessive Compulsive Disorder (OCD) Going?
What Keeps Obsessive Compulsive Disorder (OCD) Going?
Understanding Obsessive Compulsive Disorder (OCD)
Understanding Obsessive Compulsive Disorder (OCD)
Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)
Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)
Intolerance Of Uncertainty
Intolerance Of Uncertainty
Links to external resources
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
Assessment
-
Obsessive Beliefs Questionnaire (OBQ-44)
| Obsessive Compulsive Cognition Working Group | 2001
- Scale
- Obsessive Compulsive Cognition Working Group. (2001). Development and initial validation of the Obsessive Beliefs Questionnaire and the Interpretation of Intrusions Inventory. Behaviour Research and Therapy, 39, 987–1006.
OCD
- Obsessive Compulsive Inventory (OCI) scoring grid
- Relationship Obsessive Compulsive Inventory (ROCI)
- Partner Related Obsessive Compulsive Symptom Inventory
- OCD Trauma Timeline Interview (OTTI) | Wadsworth, Van Kirk,August, MacLaren Kelly, Jackson, Nelson & Luehrs | 2023
- Vancouver Obsessional Compulsive Inventory (VOCI)
Guides and workbooks
- What you need to know about OCD | International OCD Foundation (IOCDF)
- Managing obsessive compulsive disorder | Simon Enright
- Obsessive compulsive disorder: patient treatment manual | Clinical Research Unit for Anxiety and Depression (CRUfAD)
- OCD: An OCD-UK Information Guides For People Affected By Obsessive Compulsive Disorder | OCD-UK
- Self-Help: Managing Your OCD At Home | Anxiety Canada
Information Handouts
- "Just Right" OCD Symptoms | IOCDF | 2009
- What are postpartum and perinatal OCD? | IOCDF
Information (Professional)
- Scrupulosity and OCD: information packet for faith leaders | IOCDF, ADAA
Presentations
- Cognitive behavioral therapy for OCD | Sabine Wilhelm
- New directions in implementing exposure and response prevention: an inhibitory learning perspective | Jonathan Abramowitz | 2018
- Cognitive Therapy for Contamination-Related OCD: ERP and Beyond | Adam Radomsky | 2011
- Interoceptive exposure: an underused weapon in the arsenal against obsessions and compulsions | Jonathan Abramowitz | 2018
- Family affair: involving a partner or spouse in exposure and response prevention for OCD | Jonathan Abramowitz | 2018
- A couple-based approach to CBT for BDD | Lillian Reuman, Jonathan Abramowitz | 2016
- Body dysmorphic disorder | David Veale | 2017
Treatment Guide
- NICE Guidelines For OCD and BDD | NICE | 2005
- Treatment of patients with OCD | American Psychiatric Association (APA) | 2007
- Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders (2014) | Katzman et al | 2014
- A psychological perspective on hoarding – DCP good practice guidelines | Holmes, S., Whomsley, S., Kellet S. | 2015
- Treatment Manual For OCD | Clinical Research Unit for Anxiety Disorders (CRUFAD) | 2010
Recommended Reading
BDD
- Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image ,1, 113-125
OCD
- Gillihan, S., Williams, M. T., Malcoun, E., Yadin, E., Foa, E. B. (2012) Common pitfalls in exposure and response prevention (EX/RP) for OCD. Journal of Obsessive-Compulsive and Related Disorders, 1, 251-257
- Rachman, S. (1997). A cognitive theory of obsessions. Behaviour Research and Therapy, 35(9), 793-802
- Mataix-Cols, D., et al (2010). Hoarding disorder: A new diagnosis for DSM-V? Depression and Anxiety, 27, 556-572.
- Salkovskis, P. (1999). Psychological treatment of obsessive–compulsive disorder. Behaviour Research and Therapy, 37, S37-S52
- Salkovskis, P. M. (2007). Psychological treatment of obsessive–compulsive disorder.Psychiatry,6(6), 229-233
- Veale, D. (2007). Cognitive behavioural therapy for obsessive compulsive disorder. Advances in Psychiatric Treatment. 13, 438-446
- Veale, D., Freeston, M., Krebs, G., Heyman, I., & Salkovskis, P. (2009). Risk assessment and management in obsessive–compulsive disorder. Advances in psychiatric treatment, 15(5), 332-343.
BDD
- Danesh, M., Beroukhim, K., Nguyen, C., Levin, E., & Koo, J. (2015). Body dysmorphic disorder screening tools for the dermatologist: A systematic review.Pract Dermatol,2, 44-49.
- Krebs, G., de la Cruz, L. F., & Mataix-Cols, D. (2017). Recent advances in understanding and managing body dysmorphic disorder. Evidence-Based Mental Health, 20(3), 71-75.
OCD
- Doron, G., & Derby, D. (2015). Assessment and treatment of relationship-related OCD symptoms (ROCD): a modular approach. Handbook of Obsessive-Compulsive Disorder across the Lifespan. Hoboken, NJ: Wiley (Forthcoming).
BDD
- Veale, D. (2001). Cognitive-behavioural therapy for body dysmorphic disorder. Advances in Psychiatric Treatment, 7, 125-132
- Assessment and treatment of relationship-related OCD symptoms | Guy Doron, Danny Derby | 2017
OCD
- Clark, D. A., & Rhyno, S. (2005). Unwanted intrusive thoughts in nonclinical individuals. Intrusive thoughts in clinical disorders: Theory, research, and treatment, 1-29
What Is Obsessive Compulsive Disorder?
Signs and Symptoms of OCD
People with OCD experience obsessional thoughts, images, urges, and doubts. They often feel compelled to act or think in certain ways.Obsessions are intrusive thoughts—thoughts that are unwanted and unacceptable, and which pop into our minds unbidden. Obsessions can be thoughts in the form of words, but also of images (pictures in our minds), urges or impulses, or feelings of doubt. Obsessive thoughts are experienced as unacceptable, disgusting, or senseless, and people with OCD find it hard not to pay attention to them. Examples of obsessions include:thoughts such as ‘My hands have been contaminated with germs’ or ‘Perhaps I am a pedophile’
images of my family being murdered
doubts such as ‘Have I left the stove on?’
urges such as wanting to shout profanities
carefully washing food after having an intrusive thought about germs;
calling family members to check they are OK after having an intrusive image about their deaths;
going back to the house to check after doubting whether the stove was turned off;
avoiding a public place after having an urge to shout profanities.
Prevalence of OCD
The lifetime prevalence rate of OCD in the United States is estimated to be 2.3% in adults (Kessler et al., 2005), and 1% to 2.3% in children and adolescents (Zohar, 1999).Psychological Models and Theory of OCD
The cognitive behavioral theory of OCD proposes that when someone experiences an intrusive thought it is the appraisal—what they make of having the thought—that is most important (Salkovskis, Forrester, & Richards, 1998). Intrusive thoughts, even very unpleasant ones, are common and entirely normal. What seems to happen in OCD is that the fact of having intrusive thoughts is interpreted as being especially significant and, as a result, is especially anxiety-provoking. People with OCD are more likely to feel especially responsible for any potential harms and may feel especially strong emotion should they have intrusive thoughts about harm occurring. Compulsions are understood to be an active attempt to reduce harm. According to the cognitive model of OCD targets for intervention include:understanding and addressing the meaning of the intrusions;
targeting compulsions and safety-seeking behaviors;
modifying attentional biases.
Evidence-Based Psychological Approaches for Working with OCD
Cognitive behavioral therapy (CBT) is an evidence-based psychological treatment for OCD. Historically, CBT for OCD has involved the behavioral approach of exposure with response prevention (ERP). More cognitive approaches within CBT attempt to understand the patient’s appraisal of their intrusions and to find ways of exploring the validity and consequences of these appraisals.Resources for Working with OCD
Psychology Tools resources available for working therapeutically with OCD may include:psychological models of obsessive-compulsive disorder (OCD)
information handouts for obsessive-compulsive disorder (OCD)
exercises for obsessive-compulsive disorder (OCD)
CBT worksheets for obsessive-compulsive disorder (OCD)
self-help programs for obsessive-compulsive disorder (OCD)
References
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602.
Salkovskis, P. M., Forrester, E., & Richards, C. (1998). Cognitive–behavioral approach to understanding obsessional thinking. The British Journal of Psychiatry, 173(S35), 53–63.
Zohar, A. H. (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 8(3), 445–460.